Irritated skin
We’ve probably all had a skin irritation at some point in our lives. It might be a reaction to something we have touched or it could be due to an underlying skin problem, or even a sign of a skin infection.
How our skin reacts to different factors differs from person to person. You might have an obvious reaction, causing itchy, red skin or a rash. You may even have other symptoms, such as a fever.
Symptoms associated with irritated skin
There are many reasons why your skin can become irritated. It could be because you have dry skin, or your skin has come into contact with an allergen or irritant, or you develop a rash because of heat or infection. You may just have skin that is sensitive and prone to reacting to things like cosmetics.
- Itchy, burning skin
- Dryness
- Bumpy skin
- Rashy skin
- Flaky skin
- Red skin

Conditions linked to irritated skin
Irritated skin can be the result of a general cause like having dry skin, which is more common as we get older, or a specific trigger such as being pregnant. For others it may be due to a medical condition, such as atopic eczema, contact dermatitis or psoriasis. Irritated, rashy skin can also develop in response to an infection, such as athlete’s foot or chickenpox.
Dry skin
Dry skin is skin that is lacking in moisture or oils, which can lead to itchy, red and/or even painful skin. The severity of skin irritation will depend on how bad your dry skin is, depends on how bad your dry skin is. In mild cases, your skin may be a little bit red, itchy and flaky, while in moderately dry skin, these symptoms are a bit worse and you may also have painful skin. In severe cases, the symptoms can be intense, and your skin can become cracked. Your risk of having dry skin increases as you get older, or due to developing certain medical problems like an underactive thyroid or kidney disease. Read more on how to maintain a hydrated and moisturised skin here.
Pregnancy
Almost one in four pregnant women develop itchy skin, which can disrupt their sleep. Although pregnant women might develop irritated skin for the same reasons as everyone else, in some cases it’s due to specific pregnancy-associated conditions. The most common cause of itch in pregnancy is a condition called obstetric cholestasis, or jaundice of pregnancy, where the normal bile flow is disrupted, leading to bile salts being deposited in the skin. The fully cause of this condition is not known, but it normally presents as itchy skin with no rash.
Polymorphic eruption of pregnancy is another cause. This usually happens in the last three months of pregnancy and you’ll have a rash in addition to an intense itch. Although we’re not sure why it happens, polymorphic eruption might be triggered by the growing baby causing the abdomen to swell up.
Atopic eczema
Atopic eczema is a dry, inflammatory skin condition. As eczema skin doesn’t produce as much fat and oils as normal skin, it’s less effective at trapping moisture. You might find that there are times when your eczema is better and times when it is more irritated. This is known as a flare-up, and can happen several times a month. Atopic eczema usually starts in childhood, but can also affect up to 1 in 10 adults, more commonly if you also have asthma and/or hayfever.
Contact dermatitis
Contact dermatitis happens when our skin directly touches an allergen or irritant, setting-off an inflammatory reaction. There are two main types – allergic contact dermatitis, caused by an allergen, and irritant contact dermatitis, caused by a skin irritant. The main symptoms are itching, stinging, burning, tight, dry and chapped skin.
Common allergens include cosmetics, hair dyes, metals (e.g. nickel in jewellery) and plants such as sunflowers, daffodils and tulips. Common irritants include water, cleansers and plants such as mustard, spurge (e.g. poinsettias) and forget-me-nots.
Contact dermatitis is seen more often in those who are in regular contact with irritants at work – for example hairdressers, cleaners or nurses. It’s also more common if you have a family history of asthma, eczema or hayfever. In babies, nappy rash can be a symptom of contact dermatitis. Here, the nappy stops the baby’s skin from being able to breathe and the skin becomes too moist, causing the skin to break down. This makes it easy for irritant substances in the urine to trigger a contact dermatitis reaction, which is more commonly known as nappy rash.
Psoriasis
Psoriasis is another type of inflammatory skin condition where the rate at which our skin cells are renewed happens much faster than normal. The most common type of psoriasis is plaque psoriasis – with pink-red patches of skin covered in silver-white scales that can be itchy and cracked. There are times when psoriasis can flare-up and your skin is more irritated than usual, for example after an infection, intense sunlight or a period of stress. Psoriasis usually starts between the age of 10 and 35, and has been linked to other medical problems, such as diabetes, heart disease and obesity.
Insect bites and stings
Insect bites (e.g. bed bugs, fleas, midges and mosquitoes) and stings (most often from bees and wasps) can cause allergic reactions and lead to irritated, itchy skin. Although insect bites usually clear up within a few hours, it can take several days to get over a sting. If you have cats or dogs, they tend to attract fleas. Additionally, if you work/play outdoors, this can increase the chances of being bitten or stung, especially if you go out with bare, uncovered skin.
Infections
There are many different organisms that can cause skin infections, such as fungi and yeasts, bacteria and viruses. These can cause skin irritation and rashes, but you may also have other symptoms too. Some of the more common skin infections are:
Fungal skin infections. Athlete’s foot or ringworm are both caused by a type of fungus called a dermatophyte. You may have had flaky, itchy or painful skin in the past before any irritation develops. Around 7 in 10 people develop athlete’s foot during their lifetime, but its more common among teenagers. Most people with athlete’s foot have white or red itchy skin with scaly or moist skin between the toes (usually the two smallest toes)
Yeast infections. Candida is a yeast-like fungus that can grow within the skin folds, such as armpits, under the breasts, in the groin and neck creases. It can even be a complication of nappy rash in babies too. Skin will be itchy and sore and there may be pus-filled spots that are red underneath. Although the skin may also be scaly, it’s usually moist and red in the skin folds. You’re more likely to develop a Candida infection if you have poor hygiene, other medical problems (e.g. diabetes, anaemia), skin conditions (e.g. psoriasis, seborrhoeic eczema), you have a poor immune system (this includes babies and older people) or you are taking high-dose oestrogen such as in birth control.
Bacterial skin infections. These can cause your skin to become red, hot and swollen and you can develop lumps or abscesses. While most bacterial skin infections clear up on their own or with antibiotics, some, like cellulitis, can be serious and cause blood poisoning.
Viral skin infections. A red rash can be a typical sign of a viral infection, particularly in children. Common childhood viral infections include:
- Slapped cheek syndrome is caused by parvovirus B19 and causes a bright, red rash on the cheeks. Other symptoms include a mild fever, headache, sore throat, runny nose and upset stomach
- Chickenpox caused by the varicella zoster virus. It begins with a red rash/spots on the face or chest before spreading to the rest of the skin; these then blister and scab over around 5-6 days after the rash first appears
- Hand, foot and mouth disease is caused by the Coxsackie A19 virus. Alongside a fever, a rash develops over the hands, feet and mouth, which then blisters.
Heat rash
Heat rash – or prickly heat – develops when you sweat too much and it blocks sweat ducts. The type you’ll be most familiar with is where little bumpy spots appear, though they can also look like blisters. These can be intensely itchy and can often be found where your skin rubs against your clothes. It’s most common when you are in hot places, though children and babies can develop it as their sweat glands are less developed and therefore can get easily blocked.

Irritated skin triggers and factors
There are many different triggers that can irritate the skin, from everyday items in your home to the environment, both inside and outside.
Allergens and irritants
Allergens and irritants can cause your skin to flare up and become irritated. In addition to the allergens and irritants mentioned above, house-dust mites, pet dander and pollen can cause problems too. If you can, try to avoid the allergen.
How to manage:
- Some allergens are included in skincare products, so take care and read labels carefully
- As soon as possible after being in contact with the allergen, rinse with water or wash with soap – ideally a soap substitute
- Wipe surfaces with a damp cloth rather than dusting surfaces, as dusting can spread allergens into the air
- When pollen levels are high, avoid going outdoors or wear wraparound sunglasses while outside and bathe when you get home to remove pollen from your skin
- Avoid drying clothes outside when pollen counts are high
- Wear gloves when washing up, if the allergen is in cleansers and detergents
- If pets are the cause of your allergy, try and keep them outside, or limit them to one part of the house, vacuuming often and regularly washing bedding and soft furnishings
- To prevent insect bites or stings, keep covered with long sleeved clothing and trousers and try to avoid strongly perfumed products. Try to avoid wearing sandals or going barefoot outdoors
- Antihistamines can help you manage allergic reactions. Speak to your pharmacist or doctor for more information.
Cleansers
Soaps and cleansers are detergents that can remove water and fats from the skin, weakening the skin barrier. If you have dry skin, eczema or contact dermatitis, cleansers can make your irritated skin worse.
How to manage:
- Wash hands with a soap-free product – use an emollient as a substitute for soap
- Have short baths or showers, lasting less than 10 minutes, in lukewarm, not hot water
- Use fragrance-free products
- Wear cotton-lined gloves when washing up
- Always take any rings off before washing hands as soap can collect under jewellery, causing irritation
- Double-rinse clothing after washing to remove detergent traces – or use fabric balls as an alternative.
Clothing
Wearing tight clothes can cause dry skin or make it worse. Almost half of people with eczema say clothing irritates their skin.
How to manage:
- Don’t wear tight clothes, opt instead for loose clothing styles
- Wear clothes made from natural fabrics, like cotton or linen
- Wear cotton socks and gloves to help reduce sweat
- Avoid coarse wool as the fibres can irritate your skin
- Cut off labels and loose threads as these can also cause irritation.
Weather and temperature
Air conditioning, central heating or wood burners, all reduce humidity and so can dry skin out, making it itchy and irritated. Hot weather can also trigger prickly heat.
How to manage:
- Keep your house at a regular temperature to avoid overheating or extremes of temperature (18°C is ideal)
- Use humidifiers to put moisture back into the air or place bowls of water under radiators
- If possible, install radiators to heat your house rather than convection heaters
- If prickly heat is the problem, it’s best to try and avoid sweating too much. Take some time in an air-conditioned room or have a cool bath or shower. Wearing loose, breathable clothing can also help prevent sweating.
Stress
Stress can make dry skin, eczema and psoriasis worse as it triggers the production of substances in your body that can affect the skin barrier.
How to manage:
- Try relaxation techniques such as deep breathing, yoga, tai chi or meditation
- Use distraction methods such as baking, knitting, writing or painting
- Get a good night’s sleep
- Exercise regularly
- Talk to a healthcare professional if you feel you can’t manage your stress.
How to manage irritated skin
It is important to find out what’s making your skin irritated so you can not only avoid this trigger, but also ensure you find the right treatment. There are many different treatments available that can help relieve irritated skin depending on what’s causing it and how bad it is.
Emollients
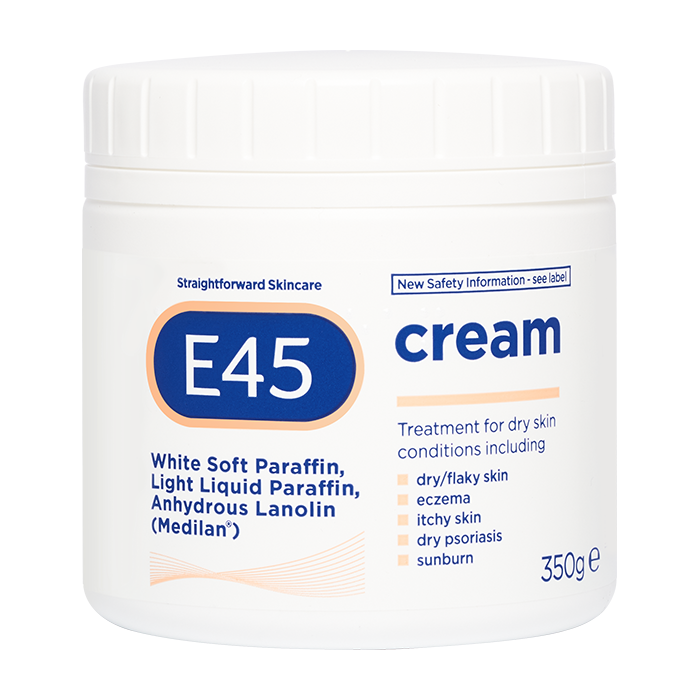
If your irritated skin is caused due to dry skin, eczema, contact dermatitis or psoriasis, then using a moisturiser called an emollient can help. In fact, if your skin is itchy, emollients are recommended as your first-choice treatment, and can also be used to ease pregnancy itch (*).
Emollients can come in many forms including creams, lotions, ointments or sprays. Emollients should be applied to the skin regularly, sometimes even multiple times a day. The area of coverage and frequency will change depending on your symptoms and condition, the severity and which product you are using. Always refer to the label for proper use. Applying emollients regularly can help irritated skin by:
- Adding and trapping moisture in the skin
- Forming a protective barrier over the skin to keep irritants and allergens out
- Helping flare-ups of conditions, such as eczema.
As regular soaps and cleansers can further irritate the skin and cause dryness, it’s also important to wash with an emollient or soap substitute. These don’t lather up like regular soap, but still do the job of getting you clean. You can also add emollients to your bath.
Some emollients contain extra ingredients that specifically target and control itchiness. These ingredients include oatmeal, crotamiton and lauromacrogols, which have a local anaesthetic action.
(*) With E45 Cream no effects during pregnancy are anticipated, since systemic exposure to white soft paraffin, liquid paraffin and lanolin is negligible. As with all medicines, this product should be used with caution during pregnancy. With E45 Itch Relief Cream there are no specific restrictions concerning its use during pregnancy, but it is not to be used on the breasts immediately prior to breast feeding during lactation.
Steroids
Mild steroids creams and ointments can be bought from your pharmacy to help relieve contact dermatitis, flare-ups of mild-to-moderate eczema and insect bites or stings. Always check the label for how to use the product correctly and safely; always check who can use the product as many over the counter steroids having limitations regarding age and pregnancy.
Note that majority of topical steroids should be applied differently to emollients:
- Apply very thinly and to just a small area
- Use once or twice a day for 7-14 days
- Apply the product sparingly to only the affected areas
Antihistamines
Antihistamines can be used to help relieve severe itch in atopic eczema, contact dermatitis and pregnancy itch. Ask your pharmacist or doctor which antihistamine is best for you.
Antifungals
Antifungal creams and ointments are available to treat athlete’s foot, ringworm and Candidal infections. Some also contain a mild steroid to help reduce any inflammation. Ask to speak with your pharmacist or doctor to determine which treatment and/or product is best for you.
Speak to your healthcare professional if:
- In addition to a rash, you feel unwell
- You don’t know what has caused the rash
- Your rash doesn’t go away quickly
- Your rash doesn’t fade when you press a glass gently against it
- Your irritated skin is affecting your daily life
- You are worried about other symptoms
- Irritation persists for more than 2 weeks, or keeps returning
- If the rash comes with a new swelling
- It’s all over your body.
Self-Care for irritated skin
Self-care can include using emollients regularly, avoiding triggers and making changes to your everyday routine.
Do
- Pat or tap your skin instead of scratching
- Wear loose cotton, breathable clothing
- Avoid known irritants
- Use fragrance-free emollients regularly – keeping them in the fridge to apply cold can also help
- Hold something cool against skin, like a damp flannel soaked in emollient, to help prevent scratching
- Take cool or lukewarm baths or showers no more than once a day
- Switch to emollient cleansers or soap substitutes.
Don’t
- Wear clothes made of coarse wool or synthetic fibres
- Have long hot baths or showers, as this can remove protective skin oils (ideally no more than 10 minutes)
- Use perfumed soaps, moisturisers, deodorants or foaming cleansers
- Scratch your skin.