Psoriasis on the face: Expert tips and effective care
Psoriasis on the face can be an extremely uncomfortable and often distressing condition. However, understanding the condition and its triggers can help in managing and reducing its impact. Here, we delve into everything from understanding what psoriasis is to how to specifically manage psoriasis symptoms on the face.
What is psoriasis?
Psoriasis, a persisting autoimmune skin condition that affects millions of people around the world and causes thick, flaky patches of skin, which form silvery-white, red or grey scales. Research indicates that approximately 50 percent of people diagnosed with psoriasis experience facial psoriasis, or psoriasis on the face.
Recognising facial psoriasis: Symptoms and signs
Identifying the signs of facial psoriasis early can be key for timely diagnosis and successful management. Although psoriasis shares some common traits, facial psoriasis tends to have distinctive features.
Signs of facial psoriasis can include:
- Red, inflamed skin: This can be the first indication of facial psoriasis. The skin on the face takes on a reddish hue and might feel warm to touch, signalling inflammation.
- Flaking: This can be the result of an overactive skin cell regeneration process. The excess skin cells, unable to shed naturally, cause noticeable flaking.
- Appearance of silver-white scales: The accumulation of dead skin cells can be a by-product of the rapid overproduction of skin cells. These scales can appear anywhere on the face, although they are often seen around the hairline and eyebrows.
The intensity of these symptoms can differ greatly, causing minor discomfort for some and significant distress for others. The impact of facial psoriasis goes far beyond physical discomfort, as the visible nature of the condition can lead to self-consciousness and impact one’s overall quality of life, causing psychological distress.
The difference between facial psoriasis and psoriasis on the body
Facial psoriasis, as the term implies, refers specifically to psoriasis that affects the face. Here are some key differences between facial psoriasis and general body psoriasis:
- Location: Facial psoriasis primarily affects areas like the forehead, the skin between the nose and upper lip, the upper lip itself and the skin surrounding the eyebrows. On the other hand, psoriasis on the body commonly affects areas like the elbows, knees and scalp.
- Skin sensitivity: The skin on the face is typically thinner and more sensitive than the skin on other parts of the body. As a result, facial psoriasis may require a gentler approach to treatment in order to prevent further irritation or damage to the skin.
- Visibility: The visible nature of facial psoriasis can be more psychologically distressing, impacting self-esteem and social interactions.
- Care: Due to the sensitivity of skin on the face, certain treatments that may be suitable for psoriasis on the body may not be suitable for the face.
Always consult with a healthcare professional or dermatologist for appropriate diagnosis and treatment of psoriasis, whether it’s located on your face or on other parts of your body.
Causes and triggers specific to facial psoriasis
Understanding the specific causes and triggers for facial psoriasis is key in order to effectively manage symptoms. These include:
- Genetics: Genetics plays a key role in determining an individual’s susceptibility to facial psoriasis. Research suggests that those with a family history of psoriasis are more prone to developing the condition on the face.
- Environmental factors: Conditions such as chilly weather and dry air can also exacerbate facial psoriasis. These conditions can lead to dry, flaky skin, which increases inflammation and itchiness. Excessive sun exposure can also trigger flare-ups of facial psoriasis as ultraviolet radiation can activate the immune system and worsen symptoms.
- Stress: Stress is a known trigger for psoriasis flare-ups, including facial psoriasis. It’s recommended to weave stress management techniques into your daily routine, such as meditation, deep breathing exercises, yoga or engaging in relaxing hobbies.
- Medications: Certain medications may exacerbate psoriasis symptoms. If you suspect a medication is triggering your facial psoriasis, consult with your healthcare provider.
- Smoking: Smoking is not only detrimental to overall health, it can also worsen psoriasis symptoms.
- Skin injuries: Skin injuries such as cuts, scrapes or sunburn can trigger flare-ups of psoriasis.
Coping with facial psoriasis: Emotional support and self-care
The journey of managing facial psoriasis can take a huge a toll on your psychological wellbeing – in fact, research shows that individuals with psoriasis may be more prone to experiencing depression, anxiety and reduced quality of life compared to those without the condition. Effective coping strategies can really help to manage the emotional impact of facial psoriasis and enhance mental wellbeing.
Build a support network
Creating a strong support network is a key strategy in managing facial psoriasis. Leaning on friends, family and support groups provides a safe environment to share feelings, experiences and challenges. These networks offer emotional support, practical advice and a sense of belonging, which can make a real difference when it comes to managing facial psoriasis.
Alongside traditional networks, online communities and social media platforms dedicated to psoriasis can be invaluable. These platforms allow individuals to connect with others who understand their struggles, share coping strategies and exchange information about effective treatments and products. One platform is the Psoriasis Association, which offers peer-to-peer support and a helpline to support those struggling with psoriasis.
Seeking professional help for emotional wellbeing
While support networks are crucial, individuals with facial psoriasis should also seek professional help to support their emotional wellbeing. Mental health professionals, such as therapists or counsellors, can provide specialised support and guidance. Therapy sessions can assist in developing coping mechanisms, managing stress, improving self-esteem and addressing underlying psychological issues related to the condition.
Treatments for psoriasis on the face
Topical treatments
Topical treatments are often the first step in managing facial psoriasis. Applied directly to the affected areas, they can help to reduce inflammation, itching and scaling.
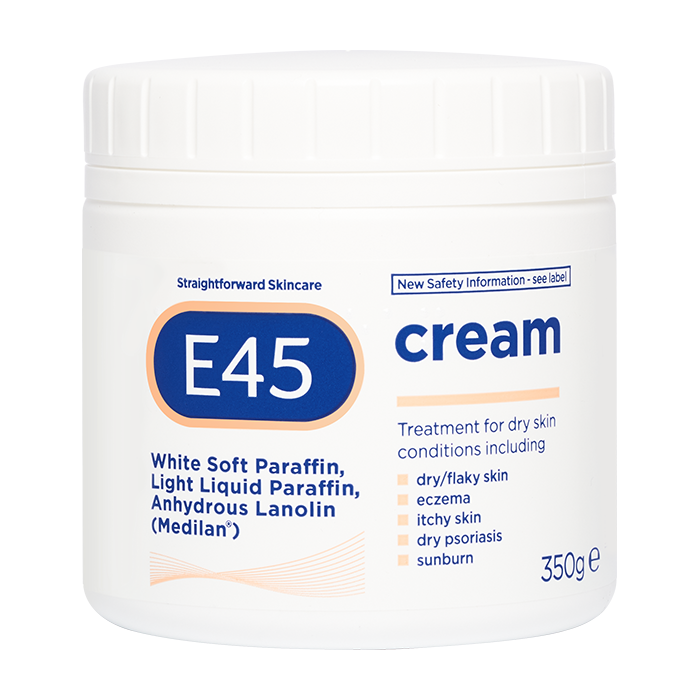
Moisturisers can play a role in managing facial psoriasis by hydrating the skin and reducing dryness and itching. They act as a protective barrier, preventing moisture loss and promoting skin healing.
Other topical treatments are available, ask a healtchare professional for advice.
Phototherapy treatment
Phototherapy involves exposing the skin to ultraviolet (UV) light to reduce inflammation and slow down the excessive growth of skin cells. It can be an effective treatment option for facial psoriasis when topical treatments alone are not enough. Consult with a healthcare proffesional to understand if this type of treatment is right for you.
Consult with a dermatologist or healthcare professional
Psoriasis on the face, and its many causes and trigger, can be a complex area, so seeking expert advice is essential. A dermatologists will conduct a detailed examination, considering the appearance, location and severity of the lesions, along with any associated symptoms. This comprehensive evaluation paves the way for a personalised treatment approach. Dermatologists can also prescribe medication and therapies that are customised to the patient’s needs.
Skincare and lifestyle tips for facial psoriasis
Managing facial psoriasis can feel like a complex puzzle, but with the correct strategies and a proactive approach, you can effectively manage flare-ups and maintain long-term control over your symptoms.
A daily skincare routine for facial psoriasis
Establishing a daily routine is essential when it comes to managing facial psoriasis. We recommend the following steps:
- Cleansing: Start your day by gently cleansing your face. Opt for a mild, fragrance-free facial cleanser that doesn’t contain any harsh chemicals which can irritate the skin.
- Exfoliating: Depending on your skin sensitivity, include a gentle exfoliation in your routine once or twice a week. This helps remove excess skin cells and can improve the effectiveness of other skincare products. Ask a healthcare professional for advice to ensure the product you are using is gentle enough.
- Moisturising: After cleansing, apply a moisturiser that’s formulated for sensitive skin. A hydrating cream or lotion can help prevent dryness and soothe irritation.
- Sun protection: Protect your skin from the sun’s harmful rays by applying a broad-spectrum sunscreen with an SPF of at least 30 every morning, and reapply as necessary throughout the day.
- Medicated treatments: If you’re using medicated creams or ointments, follow your dermatologist’s instructions. These usually go after moisturiser, but before sunscreen.
- Evening care: In the evening, cleanse your skin to remove any makeup, sunscreen or environmental pollutants from the day. Apply your moisturiser once more, and consider using a richer product or an overnight mask for added hydration.
Monitoring and managing stress levels
Stress is a well-known trigger for psoriasis flare-ups, including facial psoriasis, and so adopting effective stress management techniques can really help to manage symptoms. Techniques such as meditation, deep breathing exercises, yoga and engaging in relaxing hobbies can all help to reduce stress levels.
Maintaining a healthy lifestyle and diet
A balanced diet and regular exercise can support the immune system and reduce inflammation, helping to reduce the severity and frequency of flare-ups. A well-rounded diet should include:
- Fruits and vegetables: These provide essential nutrients and antioxidants that bolster overall skin health.
- Lean proteins: Lean proteins, like fish, poultry, and legumes, offer the necessary amino acids for skin repair and maintenance.
- Whole grains: Whole grains, such as brown rice and whole wheat bread, are packed with fibre and can help to control inflammation in the body.
Conclusion
Manging facial psoriasis can be really challenging and distressing, but with expert guidance from a dermatologist or healthcare professional, your symptoms can be managed. Adapting your daily skincare routine and making some lifestyle changes can also help. Just remember that you are not alone in this journey: there are others just like you who are struggling right now. Connecting with friends, family and others who are living with psoriasis can really help to give you the emotional support you need at this time. For more information on psoriasis in general, check out our guide to guide to psoriasis.
FAQ: Psoriasis on the face
What triggers psoriasis on the face?
Triggers for facial psoriasis can vary from person to person, but common triggers include stress, certain medications, skin injuries, smoking and environmental factors such as cold weather and dry air. Excessive sun exposure can also trigger a psoriasis flare-up.
How can I treat psoriasis on my face at home?
While professional medical advice is important, at home you can manage facial psoriasis by keeping your skin moisturised, using gentle and fragrance-free skincare products and avoiding known triggers. Sun protection is crucial, and stress management techniques like meditation or yoga can also be beneficial.
Will facial psoriasis go away?
Psoriasis is a chronic skin condition, meaning it persists over a long time. While there’s currently no cure for psoriasis, treatments can help to manage the symptoms, reduce flare-ups and improve your quality of life.
What should you not put on skin with psoriasis?
Avoid using skincare products that contain harsh chemicals, fragrances or alcohol as these can irritate the skin and exacerbate psoriasis symptoms. Always opt for products formulated for sensitive skin. If you’re unsure, consult with a dermatologist or a healthcare professional.